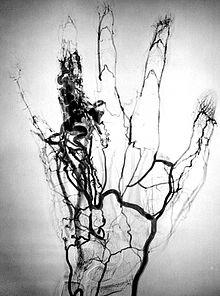
Angiography or arteriography is a medical imaging technique used to visualize the inside, or lumen, of blood vessels and organs of the body, with particular interest in the arteries, veins, and the heart chambers. This is traditionally done by injecting a radio-opaque contrast agent into the blood vessel and imaging using X-ray based techniques such asfluoroscopy.
The word itself comes from the Greek words ἀνγεῖον angeion, "vessel", and γράφειν graphein, "to write" or "record". The film or image of the blood vessels is called an angiograph, or more commonly, an angiogram. Though the word itself can describe both an arteriogram and a venogram, in its everyday usage, the terms angiogram and arteriogram are often used synonymously, whereas the term venogram is used more precisely.
The term angiography is strictly defined as based on projectional radiography; however, the term has been applied to newer vascular imaging techniques such as CT angiography and MR angiography. The term isotope angiography has also been used, although this more correctly is referred to as isotope perfusion scanning.
History
The technique was first developed in 1927 by the Portuguese physician and neurologist Egas Moniz at the University of Lisbon to provide contrasted x-ray cerebral angiography in order to diagnose several kinds of nervous diseases, such as tumors, artery disease and arteriovenous malformations. He is usually recognized as one of the pioneers in this field. Moniz performed the first cerebral angiogram in Lisbon in 1927, and Reynaldo Cid dos Santos performed the first aortogram in the same city in 1929. With the introduction of the Seldinger technique in 1953, the procedure became markedly safer as no sharp introductory devices needed to remain inside the vascular lumen.
History
The technique was first developed in 1927 by the Portuguese physician and neurologist Egas Moniz at the University of Lisbon to provide contrasted x-ray cerebral angiography in order to diagnose several kinds of nervous diseases, such as tumors, artery disease and arteriovenous malformations. He is usually recognized as one of the pioneers in this field. Moniz performed the first cerebral angiogram in Lisbon in 1927, and Reynaldo Cid dos Santos performed the first aortogram in the same city in 1929. With the introduction of the Seldinger technique in 1953, the procedure became markedly safer as no sharp introductory devices needed to remain inside the vascular lumen.
Technique
Depending on the type of angiogram, access to the blood vessels is gained most commonly through the femoral artery, to look at the left side of the heart and at thearterial system; or the jugular or femoral vein, to look at the right side of the heart and at the venous system. Using a system of guide wires and catheters, a type ofcontrast agent (which shows up by absorbing the x-rays), is added to the blood to make it visible on the x-ray images.
The X-ray images taken may either be still images, displayed on an image intensifier or film, or motion images. For all structures except the heart, the images are usually taken using a technique called digital subtraction angiography or DSA. Images in this case are usually taken at 2 – 3 frames per second, which allows theinterventional radiologist to evaluate the flow of the blood through a vessel or vessels. This technique "subtracts" the bones and other organs so only the vessels filled with contrast agent can be seen. The heart images are taken at 15–30 frames per second, not using a subtraction technique. Because DSA requires the patient to remain motionless, it cannot be used on the heart. Both these techniques enable the interventional radiologist or cardiologist to see stenosis (blockages or narrowings) inside the vessel which may be inhibiting the flow of blood and causing pain.
Uses
Coronary angiography
Main article: Coronary angiography
One of the most common angiograms performed is to visualize the blood in the coronary arteries. A long, thin, flexible tube called a catheter is used to administer the X-ray contrast agent at the desired area to be visualized. The catheter is threaded into an artery in the forearm, and the tip is advanced through the arterial system into the major coronary artery. X-rayimages of the transient radiocontrast distribution within the blood flowing inside the coronary arteries allows visualization of the size of the artery openings. Presence or absence of atherosclerosis or atheroma within the walls of the arteries cannot be clearly determined. See coronary catheterization for more detail.
To detect coronary artery disease, Computed Tomography (CT) Scan is better than Magnetic Resonance Imaging (MRI). The sensitivity and specificity between CT and MRI were (97.2 percent and 87.4 percent) and (87.1 percent and 70.3 percent), respectively. Therefore, CT (mainly multislice CT) is more accepted, more widely available, more favored by patients, and more economic. Moreover, CT requires shorter breath-hold time than MRI.
Microangiography
Microangiography is commonly used to visualize tiny blood vessels.
Neuro-vascular angiography
Another increasingly common angiographic procedure is neuro-vascular digital subtraction angiography in order to visualise the arterial and venous supply to the brain. Intervention work such as coil-embolisation of aneurysms and AVM gluing can also be performed.
Peripheral angiography
Angiography is also commonly performed to identify vessel narrowing in patients with leg claudication or cramps, caused by reduced blood flow down the legs and to the feet; in patients with renal stenosis (which commonly causes high blood pressure) and can be used in the head to find and repair stroke. These are all done routinely through the femoral artery, but can also be performed through the brachial or axillary (arm) artery. Any stenoses found may be treated by the use ofatherectomy.
Post mortem CT angiography for medicolegal cases
Post mortem CT angiography for medicolegal cases is a method initially developed by the Virtopsy group. Originating from that project, both watery and oily solutions have been evaluated.
While oily solutions require special deposition equipment to collect waste water, watery solutions seem to be regarded as less problematic. Watery solutions also were documented to enhance post mortem CT tissue differentiation whereas oily solutions were not. Conversely, oily solutions seem to only minimally disturb ensuing toxicological analysis, while watery solutions may significantly impede toxicological analysis, thus requiring blood sample preservation before post mortem CT angiography
Complications
After an angiogram, a sudden shock can cause a little pain at the surgery area, but heart attacks and heart strokes usually don't occur, as they may in bypass surgery.